What Does Your Digestion Have To Do With Your Depression?
 Depression is a very common and very enigmatic diagnosis. The cause of depression still remains to be elucidated even though 1 out of every 5 people will experience a period of depression at some point in their lives. What’s more is that most people treated for depression will experience a relapse in symptoms over a 10-year period. This prognosis does not instill confidence in the current model of treatment. The more we learn about human psychology, it seems the less we know about the human mind. To illustrate, here is a sampling of the many theories that attempt to explain the root cause of depression:
Depression is a very common and very enigmatic diagnosis. The cause of depression still remains to be elucidated even though 1 out of every 5 people will experience a period of depression at some point in their lives. What’s more is that most people treated for depression will experience a relapse in symptoms over a 10-year period. This prognosis does not instill confidence in the current model of treatment. The more we learn about human psychology, it seems the less we know about the human mind. To illustrate, here is a sampling of the many theories that attempt to explain the root cause of depression:
- Neurotransmitter dysfunction or deficiency
- Brain Derived Neurotrophic Factor deficiency
- Neuroplasticity decrease
- HPA axis dysfunction
- Inflammation and Immune system dysfunction
- Microbiota-gut-brain dysfunction
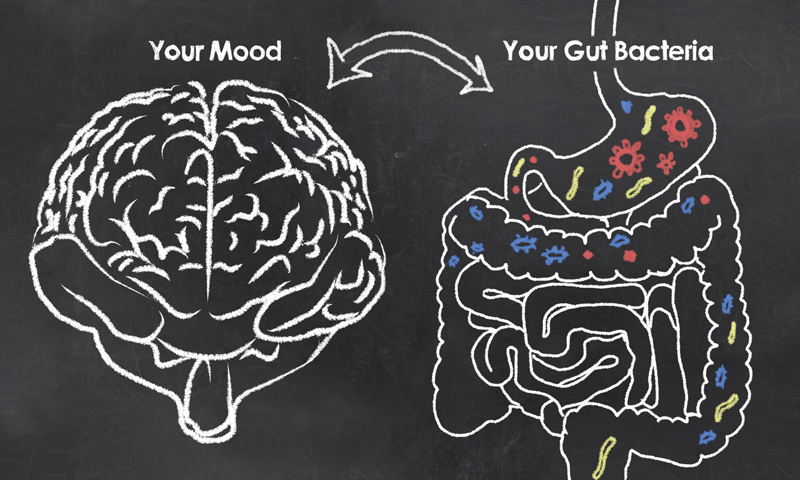
Each theory focuses on a different system as a source of the cause of depression. Does it come from the brain itself? Does it come from the HPA axis (hypothalamus, pituitary, adrenal) or is it the immune system? Perhaps the most tantalizing and most inclusive is the theory that the gut microbiome holds the majority of the power in the creation or elimination of depression. Humans have a “gut brain” that is mostly (90-95%) made up of microorganisms in our gut. These microorganisms collectively are known as the gut microbiota or microbiome. They spend their time eating what we eat and making neurotransmitters, immune proteins, and hormones. In other words, the microbiota communicate with just about every system in the body. The products that the gut microbiota make directly influence the various systems within our bodies such as the endocrine and immune system. It has been suggested that our microbiota contribute to our various body systems’ maturation. We have always looked at the body being organized in a top-down way, from brain in the head directs the rest of the body, but we are seeing evidence of the gut influencing the way the brain develops and that is really turning what we know on its head, so to speak.
What Does This Mean for Treatment of Depression?
It means that treating your gut right can make a huge impact on the way your mind and body feel. Researchers have found that the microbiome of depressed individual differs from that of non-depressed individuals. Specifically, the amount of lactic acid bacteria in depressed individuals is lower. Scientists have suggested classifying certain probiotics as “psychobiotics” that together influence psychological health. What’s more is that external factors can influence our microbiota. For example; stress, diet, and exercise all have been shown to influence the composition of the microbiota. Consider that all of these external factors are modifiable, by you, and suddenly you hold a lot of power.
To break it down:
- Ancient practices of mindfulness and meditation as well as newer practices of cognitive behavioral therapy can actually change the way our bodies and minds respond to stress. This has a direct impact on the health of your microbiome. In turn, having a healthy microbiome will actually help you cope with stress. Additionally, a dysfunctional microbiome makes you more susceptible to stress-linked disorders.
- Diet can be manipulated to increase the health of the microbiome. Using foods to support the health of the lactic acid bacteria can influence the way you feel. Supplementing probiotics can give your microbiome a boost until the new microbes become permanent residents. Additionally, including food sources of prebiotics fuel the probiotics and entice them to stay on and support your health (mental and physical).
- Antibiotic use is widespread in our current medical system. While the dawn of antibiotics heralded the decline of life-threatening infections, the current over-use of antibiotics has created “super bugs” and antibiotic resistance in the infectious organisms. Instead of using antibiotics for all ear infections, all respiratory infections, and all urinary tract infections, speak with your doctor about alternative treatments. Many upper respiratory symptoms come from viruses and the medical community is beginning to cut down on their widespread use of antibiotics for treating these conditions. In the case of a UTI, cultures of the bacteria can be obtained and antibiotics can be selected for your specific infectious bacteria.
- Exercise can be factored in to all discussions of health, both mental and physical. Implementing changes in physical activity has body-wide effects. It causes neurochemistry to change, which influences gut health in a top-down way. Increasing exercise can increase the diversity of the microbiota.
This list is just the tip of the iceberg. Entire books have been written about the effects of diet on depression. A licensed naturopathic doctor is trained to use both traditional and cutting-edge research-based medicine to treat patients with a wide variety of health concerns including digestive and mental health. The field of microbiome research is expanding daily, and the reach of the gut appears to be a lot farther than traditional gastroenterology could have ever predicted. A diagnosis of depression is not the end of the road, with proper support it can be the exciting beginning of improved overall health.
The information provided in this article is not intended to diagnose or treat any disease.
Dr. Sarah Buck is a naturopathic doctor working in Yarmouth, Maine. She was drawn to naturopathic medicine because of the ability to blend the science and art of medicine. Dr. Buck enjoys drawing upon her strong science background from her training for diagnosis and to guide her therapeutic choices. She also relishes the more creative process of working together with the patient to create a unique treatment plan. Her practice is located at 224 E. Main St.
You can find out more and book appointments at: sarahbucknd.com or call 207.200.6597.




